Approximately 300,000 babies are born with sickle cell disease each year, according to the World Health Organization (WHO).1
In the U.S., sickle cell disease affects approximately 100,000 individuals.2
Only 20% of family physicians report feeling comfortable treating people with sickle cell disease.2
The number of people with sickle cell disease is expected to grow 30% globally by 2050.2
Sickle Cell Disease Basics
Transfusion Therapy for Sickle Cell Disease
Transfusion therapy is generally defined as receiving blood via an intravenous (IV) line and is a widely utilized treatment option for specific long-term and acute complications of sickle cell disease. However, there are multiple types of transfusion therapy to manage sickle cell disease. Learn about the different types of transfusion therapy and how you may better manage your disease.3
Transfusion therapy is not the only option for treating sickle cell disease and may not be appropriate for all sickle cell disease patients. Ask the right questions when you consult your physician about whether transfusion therapy may be an option for you.
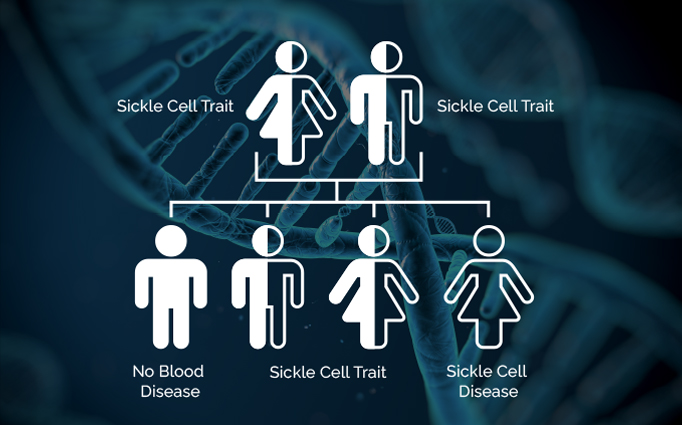
Sickle Cell Trait
People who inherit one sickle cell gene and one non-sickle gene have sickle cell trait. People with sickle cell trait usually do not have any of the symptoms of sickle cell disease, but they can pass the trait on to their children.4
Sickle Cell Disease
Sickle cell disease is a group of inherited red blood cell disorders. Healthy red blood cells are round, and they move through small blood vessels to carry oxygen to all parts of the body. In someone who has sickle cell disease, the red blood cells become inflexible and sticky and look like a C-shaped farm tool called a "sickle." The sickled cells die early, which causes a constant shortage of red blood cells. Sickled cells can also get stuck when traveling through blood vessels and clog the blood flow. This can cause pain and other serious complications such as infection, acute chest syndrome and stroke.

Why Transfusion Therapy?
Transfusion therapy is generally a safe and effective therapy for managing sickle cell disease. By giving you healthy red blood cells or exchanging sickled red blood cells with healthy ones, transfusion can allow oxygen to flow more easily through your body to help improve symptoms and reduce complications of sickle cell disease.5

