Learn about the three types of transfusion therapies to help you manage your sickle cell disease and the related complications.
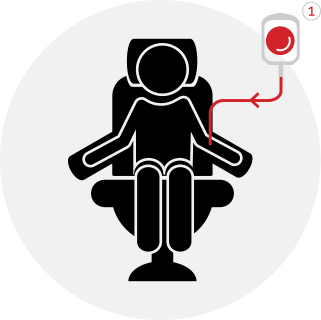
1. Simple (Also Called “Top-Up”) Transfusion
You receive a transfusion of red blood cells from a healthy donor, but none of your own blood is removed.
What to expect during the procedure
Before the procedure:
A nurse connects a blood bag containing healthy donor red blood cells to your arm through a needle.
During the procedure:
The healthy donor red blood cells flow from the bag to your body.
This requires approximately 1 to 3 units of red blood cells.
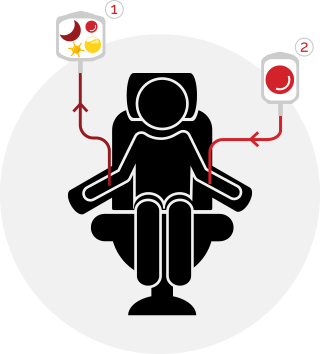
2. Manual Exchange
During this procedure, a nurse accesses one of your veins with a needle and removes a small portion of your whole blood, which contains plasma, platelets, red blood cells and white blood cells. Then a small amount of healthy red blood cells is transfused. This type of exchange is considered "manual" because an automated medical device is not required.
What to expect during the procedure
Before the procedure:
A nurse connects one vein, usually in the arm, to an empty blood bag using a needle. Another vein, usually in the opposite arm, is connected to a bag full of healthy donor red blood cells with another needle.
During the procedure:
1. The nurse draws a small amount of your whole blood, and it will flow to the empty blood bag.
2. Then the nurse transfuses a small portion of healthy red blood cells to you.
3. Steps 1 and 2 are repeated until the desired outcomes are achieved.
This requires approximately 1 to 3 units of red blood cells.
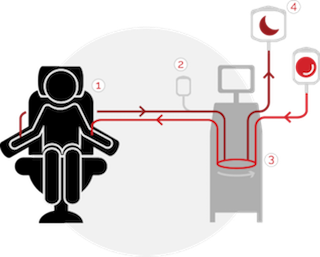
3. Automated Red Blood Cell Exchange (RBCX)
This type of exchange transfusion rapidly removes your red blood cells and replaces them with healthy donor red blood cells using an apheresis device. Not all hospitals have access to this device. This exchange transfusion requires a specialized team of trained clinicians and operators.
What to expect during the procedure
Before the procedure:
A single-use sterile tube is connected to your veins through a needle, usually in one or both of your arms. A clinician may decide that a more permanent kind of access connection is needed.
During the procedure:
1. A small portion of your blood is removed.
2. Your blood is mixed with a fluid that prevents the blood from clotting.
3. The device spins the blood in a centrifuge to separate it into red blood cells, white blood cells, platelets and plasma. At any point during the procedure, the amount of blood in the tubing set is less than the amount of cola in a can.
4. Your red blood cells flow to a waste bag and healthy donor red blood cells are returned to you along with your white blood cells, platelets and plasma.
This requires approximately 3 to 9 units of red blood cells.

How often would you need to receive the therapy?
Average procedure frequency
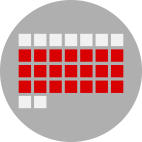
Simple transfusion
Once every 2 to 3 weeks11
Manual exchange
Once every 3 to 4 weeks6,7
Automated RBCX
Once every 4 to 6 weeks6,7

How long does each transfusion therapy procedure take?
Average procedure time
Simple transfusion
3 to 6 hours8,9
Manual exchange
2 to 4 hours6,7,8,10
Automated RBCX
1.5 to 2 hours6,7,8,9,10
What is vascular access and what kind would you need?
To provide transfusion therapy, your clinician needs access to your bloodstream. This is called vascular access or venous access, and there are several types. Peripheral venous access means that one or two needles are placed in your hand(s) or arm(s). Simple transfusion, manual exchange and automated RBCX can all be done via peripheral access in some patients.
Sometimes, a specialist will determine that they cannot access your peripheral veins and will need to place a more permanent type of vascular access device in a central vein instead of in your hand or arm.
To learn more about your vascular access options, navigate to Vascular Access Options
1World Health Organization (WHO). Fifty-ninth world health assembly. Sickle-cell anaemia: report by the Secretariat. https://who.int. Published April 24, 2006. Accessed June 1, 2020.
2American Society of Hematology. Understanding the Impact of Sickle Cell Disease. https://www.hematology.org/education/patients/anemia/sickle-cell-disease. Accessed November 5, 2020.
3Danielson CF. The role of red blood cell exchange transfusion in the treatment and prevention of complications of sickle cell disease. Ther Apher. 2002;6(1):24-31.
4Centers for Disease Control and Prevention. Sickle Cell Disease. Data & Statistics on Sickle Cell Disease. https://www.cdc.gov/ncbddd/sicklecell/data.html#:~:text=SCD%20affects%20approximately%20100%2C000%20Americans,sickle%20cell%20trait%20(SCT). Accessed June 1, 2020.
5Tsitsikas DA, Sirigireddy B, Nzouakou R, et al. Safety, tolerability, and outcomes of regular automated red cell exchange transfusion in the management of sickle cell disease. J Clin Apher. 2016;31(6):545-550.
6Dedeken L, Le PQ, Rozen L, et al. Automated red blood cell exchange compared to manual exchange transfusion for children with sickle cell disease is cost-effective and reduces iron overload. Transfusion. 2018;58(6):1356-1362.
7Kuo K, Ward R, Kaya B, Howard J, Telfer P. A comparison of chronic manual and automated red blood cell exchange transfusion in sickle cell disease patients. Br J Haematol. 2015;170(3):425-428.
8National Institute for Health and Care Excellence (NICE). Spectra Optia for automatic red blood cell exchange in patients with sickle cell disease. https://www.nice.org.uk/guidance/mtg28/chapter/5-Cost-considerations. Accessed November 2020.
9Singer T, Quirolo K, Nishi K, Hackney-Stephens E, Evans C, Vichinsky E. Erythrocytapheresis for chronically transfused children with sickle cell disease: an effective method for maintaining a low HbS level and reducing iron overload. J Clin Apher. 1999;14(3):122-125.
10Duclos C, Merlin E, Paillard C, et al. Long-term red blood cell exchange in children with sickle cell disease: manual or automatic? Transfus Apher Sci. 2013;48(2):219-222.
11Howard J. The role of blood transfusion in sickle cell disease. ISBT Science Series. 2013;8:225-228.
12Barth D, Sanchez A, Thomsen A, et al. Peripheral vascular access for therapeutic plasma exchange: a practical approach to increased utilization and selecting the most appropriate vascular access. J Clin Apher. 2020;35(3):178-187.
13Adams DM, Schultz WH, Ware RE, Kinney TR. Erythrocytapheresis can reduce iron overload and prevent the need for chelation therapy in chronically transfused pediatric patients. J Pediatr Hematol Oncol. 1996;18(1):46-50.
14Fasano RM, Leong T, Kaushal M, Sagiv E, Luban NL, Meier ER. Effectiveness of red blood cell exchange, partial manual exchange, and simple transfusion concurrently with iron chelation therapy in reducing iron overload in chronically transfused sickle cell anemia patients. Transfusion. 2016;56(7):1707-1715.
15Al-Salem AH. Medical and Surgical Complications of Sickle Cell Anemia. Springer; 2016.
16Cobianchi C, Fafoutis D, Roig J, Dierick K, Comasolivas N. Measuring health-related quality of life in individuals with sickle cell disease undergoing automated red blood cell exchange. Poster presented at: Sickle Cell Disease Association of America Annual Meeting: October 2018; Baltimore, MD.
17Barth D, Nemec RM, Cho DD, et al. The practical integration of a hybrid model of ultrasound-guided peripheral venous access in a large apheresis center. J Clin Apher. 2020; 35(4):328-334.
18Crookston KP. Therapeutic Apheresis: a Physician’s Handbook. 5th ed. Bethesda, MD: AABB/ASFA; 2017.
19AABB. Circular of Information for the Use of Human Blood and Blood Components. Bethesda, MD: AABB; 2017.
20European Directorate for the Quality of Medicines & HealthCare (EDQM). Guide to the Preparation, Use and Quality Assurance of Blood Components. 20th ed. Strasbourg, France: EDQM Council of Europe; 2020.